PSORIASIS
6 ways to manage itchy skin when you have psoriasis
If itchiness interferes with your daily routine, consider these strategies for finding relief.
People with psoriasis report persistently itchy skin as one of the most bothersome symptoms they experience. Itchiness can be painful, interfere with sleep and make it hard to concentrate at work.
If you struggle with skin itch related to your psoriasis, here are six strategies that might help you find some relief.
- Keep your skin moisturized. Dry skin is itchy and it can worsen the itch of psoriasis. Apply moisturizer daily. Use gentle soaps that won't dry out your skin. If the air where you live is very dry, use a humidifier to add moisture to the air.
- Stay cool. Being too hot can make your skin feel itchy. Use warm water instead of hot water for showers and baths. Wear light clothing if you're outside on hot days so you don't overheat. Turn on the air conditioning indoors to get a break from hot weather. Keep cold packs in your freezer and apply them to itchy spots for cooling relief. Some lotions include ingredients to create a cooling sensation, such as menthol.
- Don't scratch. Scratching provides only temporary relief from itchy skin. It actually makes your skin itchier because it activates the nerve fibers in your skin. If you find yourself giving in to the temptation to scratch, cover the area with confining clothes or a temporary bandage. Trim your nails so that they won't hurt your skin if you scratch.
- Be gentle with your skin. Wash gently, rather than scrubbing your skin in the shower or bath. Avoid harsh soaps that will dry and irritate your skin. Choose clothes with soft fabrics that won't contribute to itchiness.
- Avoid stress. Stress worsens itchiness. Take steps to reduce the stress in your life, such as making time for what matters to you and turning down additional responsibilities. Find ways to cope with the stress you feel, such as doing things you enjoy and activities that focus your mind on something other than your stresses. Consider meditation, yoga, and spending time with friends and loved ones.
- Talk to your doctor. Treating your psoriasis can help reduce the itchiness you experience. Tell your doctor how itchiness interferes with your daily activities. Together you might consider a new treatment strategy. Treatments specifically for itchiness are also available.
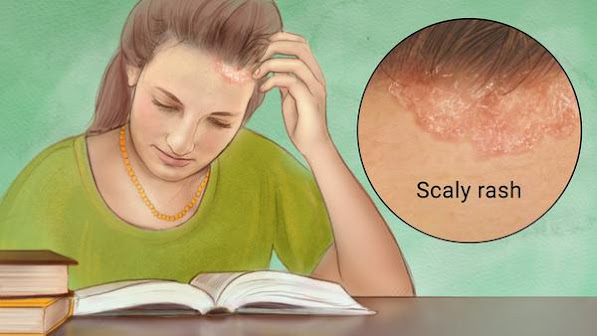
A condition in which skin cells build up and form scales and itchy, dry patches. Psoriasis is thought to be an immune system problem. Triggers include infections, stress, and cold.
The most common symptom is a rash on the skin, but sometimes the rash involves the nails or joints.
Treatment
aims to remove scales and stop skin cells from growing so quickly.
Topical ointments, light therapy, and medications can offer relief.
Very common
More than 3 million US cases per year
Treatment can help, but this condition can't be cured
Requires a medical diagnosis
Lab tests or imaging rarely required
Chronic: can last for years or be lifelong
For informational purposes only. Consult your local medical authority for advice.
Sources: Mayo Clinic and others. Learn more